Can AI revolutionize the growing, billion-dollar global market for clinical alarm management in hospitals—and help save lives?
In some intensive care units (ICUs) swamped by the coronavirus pandemic, metal poles with plastic IV lines stand sentinel in the hallways with their special-order, six-foot-long wires and tubes snaking into people’s rooms and plugging in to sensors that monitor their vital signs while delivering intravenous treatments.
Normally, intravenous fluids would be safely tucked in the same room as the person receiving them but pulling these setups out into the hallways instead allows doctors and nurses to manage some alarms and medicines without entering a patient’s room every time an alarm goes off. The combined volume of alarms, cell phones, air conditioners, and other machinery in some hospitals has been known to reach nearly 100 decibels, a noise level comparable to having a jackhammer in the middle of the ICU.
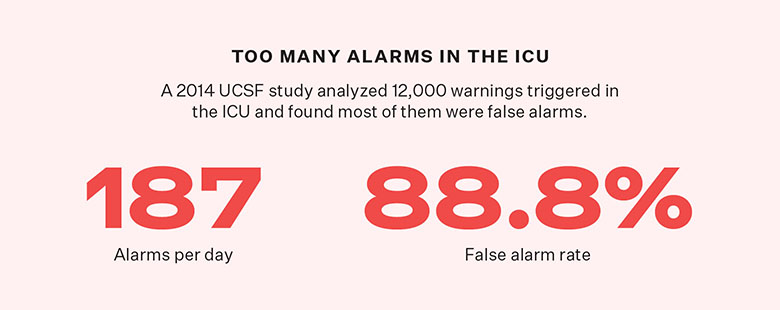
The pandemic added a new layer of complexity to the long-existing problem of alarm fatigue—a situation in which there are so many alarms in hospitals that nurses become numb to their shrieks, ignore them, or even turn them off outright (any of which can spell doom for patients). In 2014, Barbara Drew, a nurse and researcher at the University of California, San Francisco, published a study demonstrating that on average, anyone admitted to the ICU triggers 187 alarms per day, most of which are false. In the case of heart arrythmias, nearly 90 percent of the more than 12,000 alarms her team analyzed were false positives. The people whose vitals triggered the alarms actually were fine in the overwhelming number of cases.
When COVID-19 began filling U.S. emergency rooms a year ago, the stakes of responding to hundreds of false alarms became much higher. To rush into a patient’s room, a nurse would have to don fresh personal protective equipment (PPE), which was problematic in early 2020 while the nation faced a shortage of such gear. To enter every room for every alarm would cause a hospital to quickly run out of clean PPE. But the alternative was worse: To enter a room without such precious PPE protection would put employees at high risk of contracting—and spreading—the deadly virus.
COVID-19 has “created a different kind of tension,” says Josh Winowiecki, a nursing graduate student and clinical instructor at Michigan State University. It “renewed the urgency,” of managing hospital alarms, he says, and a growing movement in the field is seeking to develop solutions with the help of artificial intelligence. Researchers are building AI algorithms they hope will integrate readings of many separate vital signs to give practitioners a simple and accurate snapshot of a person’s condition. “In the past, a hospitalized patient may have had six measurements done in a day. Now we do 96,” says Thomas Hale, chief medical officer of Virtusense, a company working on new monitoring solutions.
The hospital room of the future
When alarm fatigue started gaining national attention after notable patient deaths in 2011, nurses were initially blamed. They were accused of turning the alarms off and for faulty practices that contributed to excess alarms to begin with, like improperly placing skin electrodes that triggered alarms when they needed to be adjusted or replaced. A decade later, it’s become clear that the problem is not with the nurses, their work, or with the sticky halves of skin patches, but with the alarm systems themselves. And COVID-19 has made this even more apparent. “I don’t think this is entirely a nursing problem,” says Michele Pelter, another nurse–researcher who trained under Drew and took over for her at UCSF when she retired in 2014. “What we’ve learned is that algorithm deficiencies are driving the vast majority of these alarms.”
In order to be accredited, an ICU must demonstrate that it has certain equipment with functional alarms such as ventilators that can alert practitioners if oxygen supply is too low. “Alarms are a key element of the ICU,” says Tobias Merz, a senior medical consultant at the Auckland City Hospital ICU in New Zealand where COVID-19’s spread has been minimal. But over the years, the number of alarms has grown, with each machine capable of sounding many alerts. Pelter herself helped introduce a new alarm in the 1990s to detect heart attacks.
In 2018, the global market for clinical alarm management was estimated to be $457 million, but by 2023, that number is expected to triple to $1.7 billion. A MarketsandMarkets report suggests that the need for increased accuracy and fewer alarms is a main factor in driving that increase.
“You only have a couple of minutes to do your decision making. So we, in medicine, have to find a solution.”
Hale and Pelter have remarkably similar views of the hospital room of the future. A single wire would be attached to a patch on someone’s body. That patch would contain sensors capable of simultaneously recording a slew of vital signs like heart rate, blood oxygen, and core temperature—data that would be fed into a computer that would trigger an alert if and only if that person’s medical condition actually starts to decline. The key is that the alarm wouldn’t just fire if any one vital sign blips. Pelter imagines a screen that could show a trend line demonstrating how that person’s condition has progressed since their arrival, rather than a single measurement like their current heart rate. AI would learn to detect patterns and recognize truly important changes in the patient’s condition based on the multiple inputs.
In Hale’s version, a mounted camera would view the person’s room, differentiate between patients, visitors, and health workers, and push alarms directly to nurses’ cell phones, which would give them the option to tap into the video feed and evaluate the situation remotely.
Currently, his research team is testing such a setup using data from previously hospitalized patients with known outcomes. The next step will be testing it on real people in a clinical setting.
Risk scores to the rescue
Pelter and other researchers like Merz are taking a more stepwise and hands-on approach. In March 2020, after five years of work, Merz and his team reported they’d developed an algorithm using artificial intelligence that reliably predicts circulatory failure—a situation where the blood pressure drops so low that it can permanently damage organs. His team is now working on algorithms to predict other emergencies like kidney failure and lung failure. Soon he hopes to test them all in a clinical trial.
“One big problem that we have as doctors is there’s a huge amount of information about patients. And this information is on all sorts of different systems,” says Merz. “You only have a couple of minutes to do your decision making. So we, in medicine, have to find a solution.”
Merz envisions a screen where the data from the patient monitoring systems as well as electronic health records could be integrated to form “risk scores” that would be continually updated to help physicians make those decisions.
His team isn’t alone in working toward such a goal. In January, researchers in New York developed a COVID-specific algorithm that ranks a patient’s likelihood of experiencing respiratory failure over the next 48 hours. But there’s a drawback. The risk score, which is based on electronic health records and vital signs, doesn’t replace other alarms. In fact, it can act as an additional alert. The risk score allows health care providers to “keep a closer eye on a specific group of patients that really need close monitoring,” says Theodoros Zanos, a neural and data scientist at the Feinstein Institute for Medical Research and a senior author on the study.
AI-driven approaches may be flawed if they’re trained on bad data full of false alarms.
Meanwhile, Pelter and her team are raking through millions of pieces of data one by one to identify alarms that are truly superfluous. For example, in many hospitals, an alarm sounds if a patient experiences an accelerated ventricular rhythm, because common knowledge suggested that this type of arrythmia might be a precursor to more dangerous arrythmias. But after going through thousands of alarms, her team found that the accelerated ventricular rhythm never once led to a more dangerous arrythmia. “Just because we can alarm for a particular arrythmia doesn’t mean we should,” Pelter says.
The solution to alarm fatigue “starts with good data” says Pelter. AI-driven approaches may be flawed if they’re trained on bad data full of false alarms.
Zanos agrees. “The quality of the data definitely determines how good your algorithm is,” he says. “We’re not doing this as an academic exercise. We need to speak to the stakeholders… the clinicians, the physicians, and the nurses. We really need to understand what the real issues are, and not just be creating algorithms just to create the algorithms.”